“ACA risk adjustment management: Going all-out” is the first article in the risk adjustment management series and should be read before the remaining three articles.
Although aspects of the risk adjustment puzzle in the Patient Protection and Affordable Care Act (ACA) marketplace have proven difficult to solve, its potential impacts have been known since the announcement of the first transfer payments in the summer of 2015. As a rule of thumb, we generally equate a one basis point (0.01) increase in a member’s risk score for a typical ACA issuer to a $2 to $3 per member per month (PMPM) rise in the risk transfer benefit attributable to that member.1 And, given that the average risk score of the least severe conditions in the 2017 ACA model is almost 0.70 —or 702 times more than the benchmark—it becomes immediately apparent how significant any movement in the risk score can be.
Coding completeness (CC) is a broad strategy to achieve and maintain higher levels of coding accuracy supported by more comprehensive and complete medical record documentation. As we close the ACA’s fourth benefit year, we find many issuers still do not pursue opportunities to more precisely reflect their risks through CC activities. For other health markets, there has been a sizable incentive to do so ever since the introduction of the first risk adjustment models to calculate Medicaid capitation rates and, later, Medicare Part C and Part D reimbursements. 3,4 As a result, carriers familiar with these programs have a history with these techniques.
In this topic-specific paper in our series on ACA risk adjustment management,5 we address strategies to facilitate an organizational CC initiative and “crack the code” on the tools and methods for increasing the program’s success.
Framing the approach
A comprehensive CC approach is a multifaceted, year-long initiative. It should be a corporate goal, integrated into an issuer’s compliance program. The table in Figure 1 shows a sample timeline for benefit year 2017.
Figure 1: Sample CC Timeline for Benefit Year 2017
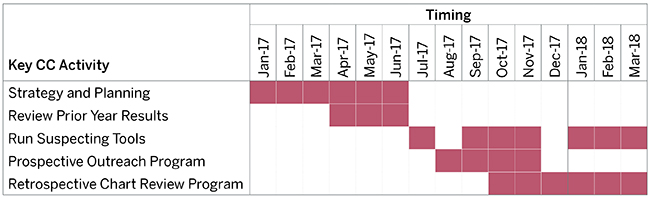
The process starts with planning current-year activities and evaluating the outcomes from prior efforts. Effective planning serves to align resources, develop long-term road maps and action plans for upcoming tasks, and, most importantly, establish ownership. CC initiatives lacking organization and clear accountability will, unsurprisingly, fall short of interim targets and overall operational goals. We also recommend a full evaluation of the program annually, including written assessments of performance and revisions based on feedback and new objectives.
In the sections that follow, we break down the key aspects of the process and the techniques we have found most helpful in developing a robust and sustainable solution.
Deciphering the process
Components of coding completeness
A comprehensive CC includes four phases outlined in the graphic in Figure 2.
2. Retrospective
3. Data submission
4. Risk score verification
Figure 2: Phases of the CC Process
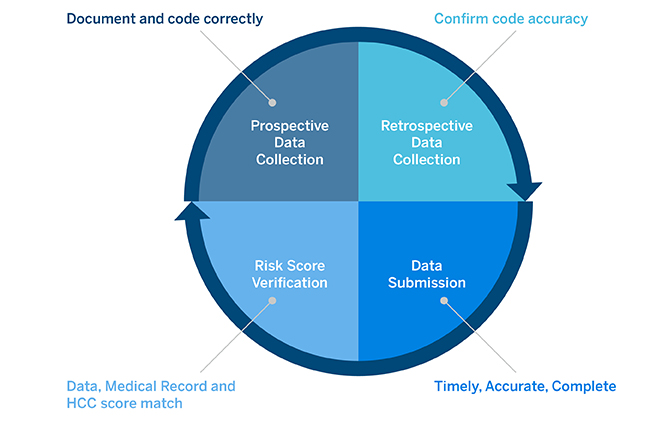
This paper primarily focuses on the prospective and retrospective phases, which require lists of members with known or suspected conditions. While a nascent program will derive the most value from retrospective chart reviews, a seasoned health plan can ease its retrospective burden by supplementing with prospective activities to increase the comprehensiveness of documentation up-front. Some of the more common prospective efforts include:
- Member outreach encouraging wellness and annual check-ups and promoting care management programs: Typically, better results are correlated with specific incentives tied to member action (e.g., medication adherence or completing an annual check-up).
- Integration of member targeting into provider electronic health records (EHRs): This strategy increases documentation comprehensiveness and quality at the time of the encounter, curbing retrospective chart review costs. Real-time provider-driven documentation and coding is almost always preferred over retrospective CC activities.
- Mobile clinics or at-home wellness assessments, if appropriate: In-person encounters will improve documentation and coding accuracy but typically come at a high price. Many individuals targeted for these encounters may seek medical services later in the year or might not have relevant diagnoses. These limitations could make the effort difficult to justify in the commercial market unless pursuing only those members with the highest likelihood of a significant uncoded medical condition.
- Provider education and incentive programs: Engaging providers to accurately document all active diagnoses is challenging, as provider reimbursement traditionally relies on the procedures and services billed and not the patient’s diagnoses. Provider engagement initiatives might include payments or bonuses for performing annual wellness visits with comprehensive medical record documentation and coding completeness—e.g., monitoring, evaluating, assessing/addressing, and treating (MEAT) documentation—or timely responses to requests to pull charts. Issuers might also include disincentives where a retrospective review identifies coding errors not supported by the documentation or general documentation inadequacy. Apart from incentives, provider education is essential, and issuers should, to the extent possible, equate coding accuracy with improved patient and provider outcomes. Prospective provider documentation and coding education also reduces the risk of identifying inaccurate codes not supported by the medical record documentation, requiring correction retrospectively.
Issuers seem to get the most traction when CC activities are performed throughout the benefit year, continually evaluating and refining the interplay between both prospective and retrospective efforts. This prevents a scramble at year-end to fit all activities into an incredibly compressed timeframe. It also ensures prospective efforts get proper attention. Continually “fixing” issues on the back-end through chart reviews will not yield the best long-term results compared to educating providers on documentation and coding best practices and working to develop plans to ensure that high-risk member conditions are comprehensively documented and accurately coded in annual visits. CC efforts can begin as early as July with targeted prospective campaigns, which tend to wind down near the close of the benefit year when all medical services must be performed. Retrospective efforts can and should continue until final EDGE server data submissions are due (in late April or early May) to ensure inclusion of the greatest number of supplemental diagnoses.
Technology and analytics
Interventions are typically informed by a "target" list of members with high likelihoods of having incomplete or inaccurate diagnosis coding, many of whom would also benefit from care management programs. These lists should include both members who are suspected of being underdiagnosed as well as those incorrectly diagnosed with conditions they do not have. The accuracy of the target list, particularly in the ACA market, is critical given the relatively low frequency of health conditions.
The most robust lists harness statistical algorithms, which synthesize data from multiple sources—member demographic information, medical procedures, pharmaceutical use, specialist visits, care management data, and socioeconomic indicators—and provide outputs in a format most useful to the professionals spearheading the CC efforts. Some analytics packages incorporate natural language processing (NLP), which identifies trigger words and phrases in EHRs to assess potential gaps in diagnosis documentation or coding. While NLP cannot be the basis for adding or removing medical record diagnoses, it can highlight potential deficiencies in charts. Having access to the best member target list can be the differentiator in achieving a positive return on investment (ROI) on CC efforts. Thus, issuers lacking the advanced analytical capabilities should consider third parties with a record of expertise in this area.
Issuers often do not place enough emphasis on assessing the value of CC outcomes. Program evaluation should include a cost-benefit analysis of all prospective and retrospective efforts as well as a top-down review of the actual activities performed during the year. A variety of clinical improvement, utilization management, and coding programs continuously compete for clinical time, administration dollars, and analytical resources. Understanding how each investment translates into a return is a necessary step in ensuring program longevity.
Over time, analyzing results can highlight notable gaps or provide metrics to benchmark or improve the process.
- Trimming target lists to only members still requiring intervention
- Algorithm refinement—either in model construction or data training techniques
- Prioritization for prospective and retrospective reviews (e.g., specific conditions, members with multiple conditions, members without any claim histories, specific providers or specialties)
- Incremental risk score increases from chart reviews or health assessments
- Value of members with no previous medical encounter versus those acquiring frequent medical care
- Identification of specialties or conditions in which a chart review is most effective
- Identification of conditions frequently miscoded, requiring addition, deletion, or more specificity
- Identification of providers consistently miscoding members
Informing the CC process with analytics will invariably improve the results. As such, measuring outcomes should not be an afterthought—something executed only when convenient. Robust CC programs place them on equal footing with the revenue-generating activities and refresh them after every campaign. While evaluation at a minimum should include ROI calculations, tracking feedback from doctors, coders, and other clinicians on the front line could provide irreplaceable insight (such as identifying miscoded condition severity levels, resulting in opportunities for focused provider education).
The teams involved
In Figure 1 above, we presented a basic representation of the key CC activities and timing. In reality, the breadth and depth of the resources are quite extensive and span more than just the analytics and finance functional areas. Figure 3 lists the major stakeholders involved throughout the CC process:
Figure 3: Key CC Stakeholders
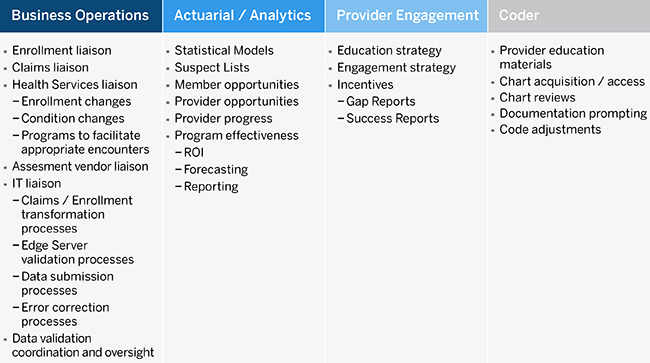
Marketing, legal, compliance, quality assurance, and member services functions also play key roles in CC activities and oversight. While organizational players shoulder responsibility for overall management, vendors and other third-party organizations specialize in all aspects of the CC value chain, including chart retrieval and medical record reviews, member list generation, EHR integration, in-home assessments, and overall process analytics. For issuers requiring assistance in one or more of the pieces, a carefully selected partner can ease internal burdens while achieving a level of expertise and performance unmatched by current staff.
Ultimately, no matter how broad its reach, CC initiatives should have one owner responsible for overseeing the process, gaining buy-in from senior leadership and department heads, planning key activities, coordinating between departments, and guiding priorities. Without such a centralized role, the myriad of individuals involved will be hard-pressed to function as a cohesive unit, and the program will suffer as a result.
Puzzle solved
Coding initiatives are investments commercial health plans will more strongly consider as the ACA moves forward. An issuer actively working to optimize its risk score position can have a material impact on its own risk transfer and will, at least to some degree, affect the transfers of all other market participants.
A health plan can leverage a variety of tactics to solve the puzzle, and no one initiative needs to follow a set template. Still, most strategies will encompass provider incentives and engagement, member outreach, EHR integration, and retroactive chart reviews at different stages of the process. On the surface, coding completeness seems like a rather narrow initiative. However, after cracking the code, it can play a key role in accomplishing incredibly important company goals to improve member outcomes, generate higher revenue, and even lower premium rates.
1Based on a simplified aggregate analysis of a member in an average rating region covered by a standard silver plan with a 1.75 market level plan liability risk score (PLRS).
2Conditions with the five lowest adult silver risk scores pulled from the 2017 CMS DIY tables, available at: https://www.cms.gov/CCIIO/Resources/Regulations-and-Guidance/Downloads/DIY-Tables-7-12-2017.xlsx.
3Pope, G.C. et al. (March 2011). Evaluation of the CMS-HCC Risk Adjustment Model: Final Report. Retrieved November 6, 2017, from https://www.cms.gov/Medicare/Health-Plans/MedicareAdvtgSpecRateStats/downloads/evaluation_risk_adj_model_2011.pdf.
4Martin, K.E. et al. (January 2004). Health-Based Risk Assessment: Risk-Adjusted Payments and Beyond. Academy Health. Retrieved November 6, 2017, from http://www.hcfo.org/files/hcfo/riskadjustment_1.pdf.
5
http://www.milliman.com/insight/aca-risk-adjustment-management-going-all-out
http://www.milliman.com/insight/ACA-risk-adjustment-management-Higher-EDGE-ucation
http://www.milliman.com/insight/aca-risk-adjustment-management-time-to-keep-score